This post’s subject is the operation of pulmonary ventilator or respirator, for treating pacientes with COVID-19 or Corona virus.
Breathing process
The muscles which act in this process are: Diaphragm and intercostal muscles, the later are between ribs.
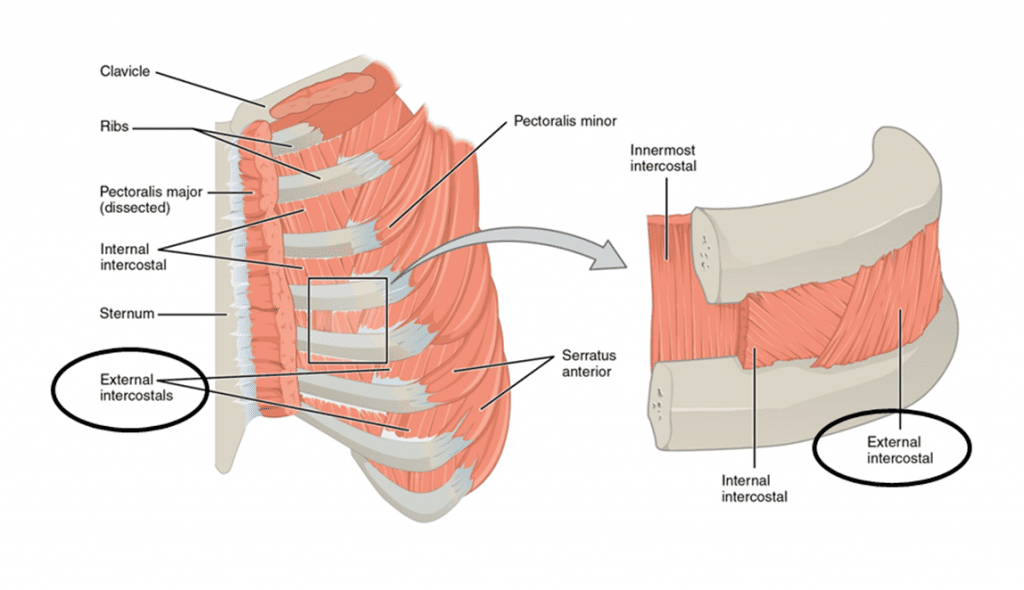
During inspiration, diaphragm and intercostal muscles contract, increasing lungs’ volume and reducing their pressure, allowing air entrance. In expiration, lungs’ volume is reduced with relaxation of diaphragm and intercostal muscles. Therefore, pressure becomes higher than the atmospheric.

Gas exchange happens in capilar vessels and pulmonary alveoli, which are very thin and flexible sacks. The excess of carbon dioxide (CO_{2}) in blood produces a toxic acidity for cells. 70% of CO_{2} in blood is in shape of bicarbonate ion (HCO_{3}^{-}), 7% is dissolved in plasma and 23% is in carbamino-hemoglobin (Hb\cdot CO_{2}). When venous blood arrives at alveoli, occurs the called pulmonary hemostasis.


Pressure of CO_{2} in blood is higher than inside alveoli. Therefore, CO_{2} dissolved in plasma enters in alveoli by diffusion and the another part separates from hemoglobin. Bicarbonate ions enter in red cells to form carbonic acid, the later degrades in CO_{2} and H_{2}O to enter in alveoli.
CO_{2}+H_{2}O\rightleftharpoons H_{2}CO_{3}\rightleftharpoons H^{+}+HCO_{3}^{-}
Meanwhile the oxygen, 98.5% join with hemoglobin forming the following reaction.
Hb+O_{2}\rightleftharpoons HbO_{2}
Rest of oxygen is dissolved in plasma.
COVID-19’s breathing problem
What happens with patient with COVID-19, assuming he isn’t healthy enough to resist the virus? Virus infects alveoli, generating immunological response which causes inflammation. Therefore, alveoli’s interior is in a fluid which makes gas exchange harder.

Inflammation also can affect bronchi and bronchioles. This is a video from George Washington University Hospital, showing lungs with COVID-19. Damaged parts are in green and yellow.
Operation of pulmonary ventilator for COVID-19
Now let’s go to electronic part. Function of pulmonary ventilator is to bring oxygen and take carbon dioxide from patient. A plastic bag is squeezed regularly by a mechanism, whose frequency is controlled electronically.

Tube which guides air to person can be non-invasive, with a mask, or invasive, tube put in trachea, depending on person’s situation.

Barotrauma and volutrauma
These are colateral effects of breathing with pulmonary ventilator. Barotrauma is a lesion in pulmonary tissue caused by excessive pressure. Ventilator operates in a frequency which does not depends on person, consequently, can become uncomfortable. If don’t enter in synchrony with diaphragm and intercostal muscles, will increase pressure in alveoli, could cause inflammation and rupture. Volutrauma is injure caused by overdistension of alveoli. Patients with COVID-19 are more subjected to these injuries.
Pulmonary ventilator control
Just injecting air in a frequency range isn’t enough. It is necessary to regulate air flux with a closed loop control system. A sensor which detects electrical activity in diaphragm, pressure and air flux sensors are necessary for air control.

Other components

Air flux to patient is controlled by valves. The later need a fast microcontroller to respond to body reactions in right time. Blender serves to air get the right quantity of oxygen. Before enters in the person, air needs to have a filter to stop bacteria, be humidified and warmed to avoid damages to pulmonary tissue. Because of that, have humidifier and nebulizer.



